An estimated $1.7 trillion is spent annually to treat these diseases in Europe and the US alone.1,2 And, as these conditions often profoundly impact the lives of patients by impairing cognitive function, mobility and overall well-being, the urgent need for effective remedies is undeniable. However, the drug discovery process for neurological conditions can be challenging. Currently, approximately 85% of central nervous system (CNS)-targeting drug trials end in failure.3 The disparity seen between the results observed in preclinical models and final clinical outcomes highlights the need for drug developers to come up with novel approaches to neurological drug discovery.
One such method is based on the integration of human induced pluripotent stem cells (iPSCs) into in vitro screening workflows. iPSCs can differentiate into a variety of cell types in the brain. Notably, they also act as a physiologically relevant and human-specific model system that can be used in drug development to bridge this gap. By providing access to patient-derived cells, while also overcoming the challenges of tissue inaccessibility, iPSCs could play a pivotal role in neuropharmaceutical drug development.
iPSCs act as a physiologically relevant and human-specific model system
Understanding the challenges
Neurological drug discovery faces a range of unique challenges, with one of the most formidable obstacles being the blood-brain barrier (BBB). This protective layer surrounds the brain and regulates the entry and exit of substances. And although it’s essential to maintain a stable brain environment, this barrier poses a significant hurdle to drug delivery. Many promising compounds fail to effectively cross the BBB and reach their intended target(s) in the CNS, ultimately limiting their therapeutic potential.
Furthermore, ensuring a drug’s adequate bioavailability is also essential, which is often influenced by the natural physiological barriers that protect the brain. Additional factors such as drug metabolism, efflux pumps and protein binding can further reduce a drug’s ability to reach its intended destination in the brain, which can significantly impact its efficacy. In some cases, this may necessitate the use of higher doses, which can enhance the active ingredient’s associated safety and toxicity risks.
Another critical challenge lies in the inaccessibility of human brain tissue. Getting this material for research, if not challenging, is often impossible. This limits the development of accurate disease models while also hindering the direct evaluation of drug efficacy in human brain tissue.
iPSCs: a solution to drug development challenges
Although there are many hurdles to overcome when developing a drug product for neurological diseases, iPSCs are emerging as a powerful tool to address these challenges. For example, they: 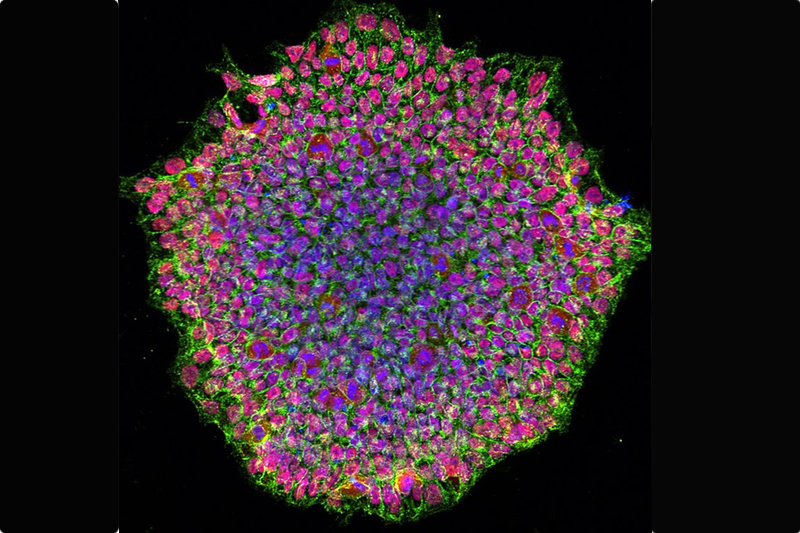
- provide human-specific and physiologically relevant model systems that improve their predictability
- power preclinical studies
- enable the study of human-specific disease mechanisms and drug responses
- overcome the limitations of tissue inaccessibility by providing access to human brain cells
- enhance reproducibility and scalability with automation and standardised protocols when used with modern laboratory techniques — allowing for high-throughput testing and compound library screening
- offer an ethically sound alternative to embryonic stem cells
- allow drug developers to screen their candidates for BBB-crossing potential while also evaluating efficacy and safety early in the development process.
Drug discovery trends that are driving progress
Alongside iPSC technology, there are a few emerging trends that could be key in the field of drug discovery.
Genetics: With the increasing availability of genotypic and phenotypic data, as well as advancements in bioinformatics, target identification/validation is becoming easier and more efficient than ever before. By unravelling the genetic underpinnings of neurological diseases, researchers can pinpoint specific genes and pathways that contribute to disease onset and progression — potentially leading to the discovery of novel drug targets. iPSCs are then available as a unique platform to validate these genetic targets as they allow drug developers to study the functional consequences of mutated iterations in a human-relevant model system.
Cellular mechanisms: A deeper understanding of the cellular mechanisms behind neurological disorders such as Alzheimer’s is increasingly emerging. As iPSC technology enables researchers to generate a variety of neural cell types, their cellular mechanisms can easily be studied. By targeting these shared mechanisms with iPSC-derived models, researchers can pursue disease-agnostic approaches — potentially developing drugs with broader therapeutic applications. This approach not only streamlines drug development but highlights whether it may be possible to treat multiple neurological conditions with a single therapeutic agent.
Using biomarkers to guide drug development: Translational biomarkers are playing an increasingly vital role in drug discovery for neurological diseases. iPSC-derived cells can be used to develop in vitro assays that measure these biomarkers, providing a platform for drug screening and validation. By utilising advanced imaging techniques or measuring drug levels in the cerebrospinal fluid, researchers can access valuable insights into drug action within the human brain; this can be complemented by iPSC-based assays to assess a drug’s effect on cellular function and disease-relevant pathways.
Additionally, identifying and validating blood-based biomarkers is a less invasive and more accessible way to monitor disease progression and treatment response, facilitating patient stratification and improving clinical trial design. As iPSCs can aid in the discovery and validation of such biomarkers, they can be key to optimising the clinical research process.
Adoption (of iPSCs) requires researchers to address ... cell production, differentiation and screening
Scaling-up the use of iPSCs
For iPSCs to have a positive effect on drug discovery, they must be successfully implemented at scale. Although the advantages of iPSC-derived models are clear, their widespread adoption requires researchers to address practical considerations, such as cell production, differentiation and screening. Advancements in automation and standardisation are crucial in this regard as they minimise the impact of human error and enhance reproducibility — ensuring the efficient and reproducible use of iPSCs in drug discovery workflows. 
Standardised protocols ensure consistency throughout experiments, further improving the reliability of data generated from iPSC-based assays. High-throughput screening capabilities, coupled with the strategic selection of compound libraries using computational chemistry and bioinformatics, allows for the rapid and efficient testing of large compound libraries; this increases the chances of identifying promising drug candidates.
iPSCs at the forefront of innovation
As iPSC technology continues to advance, its integration with other emerging trends has the potential to reshape the drug discovery landscape. Utilising such cell types could play a central role in the following applications.
- Homogenous clinical trials: Utilising iPSC models allows researchers to screen for drug responses in cell lines with specific genetic profiles or disease subtypes. This will subsequently help them to identify effective compounds in specific patient subsets. The identification and validation of genetic subtypes and other biomarkers within diseases impacted by multiple factors enables the design of more targeted and personalised clinical trials, potentially increasing success rates by focusing on specific patient populations with shared pathological characteristics.
- Computational chemistry driven methods: The combination of computational modelling and iPSC-derived data can significantly accelerate drug discovery. By leveraging the power of computational tools, researchers can predict the interactions between potential drugs and their targets in iPSC-derived cells, guiding the selection of compounds for further testing and reducing the reliance on costly and time-consuming experiments.
- Cocultures and organoids: The development of more complex in vitro models, such as cocultures and organoids, allows for a more accurate elucidation of the brain’s cellular microenvironment. iPSCs are essential when it comes to generating the diverse cell types needed for such models.
A new approach to drug discovery
By offering a human-specific, physiologically relevant and scalable system, iPSCs are uniquely positioned to overcome the challenges associated with traditional models. Through the integration of iPSC models into in vitro screening workflows, drug developers can expedite the development of much needed novel therapies for neurological conditions.
As research progresses, we can envision a future wherein the complexities of the brain are better understood, leading to the creation of targeted and effective treatments that can significantly improve the lives of individuals with neurological diseases. The journey may be challenging but the potential rewards are notable.
[Photo credit: Daniel Soñé Photography, LLC, National Eye Institute]
