Patients suffer from pain and stiffness in the joints. In severe cases, joint replacement may be appropriate.
Otherwise, treatment largely relies on pain relief. A new potential treatment, lorecivivint, is being investigated by San Diego-based biotech Biosplice in osteoarthritis of the knee.1
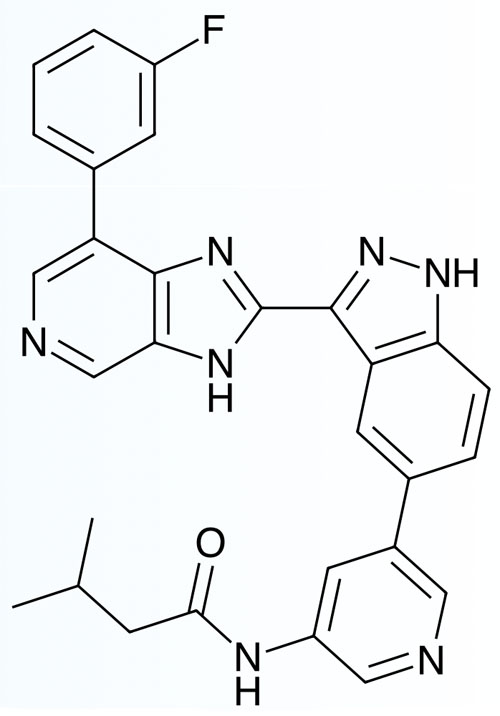
When upregulated, the Wnt signalling pathway contributes to OA and lorecivivint modulates this cascade by inhibiting the kinases CLK2 and DYRK1A, a tactic that may prove to be disease modifying.
Several clinical trials have been done on the molecule, including a Phase IIa proof of concept study.2
In the 52-week multicentre, randomised, double-blind, placebo-controlled dose-ranging trial, 455 subjects with OA of the knee were given a single 2 mL intra-articular injection containing 0.03, 0.07 or 0.23 mg of lorecivivint or a placebo.
Although the primary endpoint of a significant improvement in the WOMAC pain score compared with the placebo at week 13 was not met by any group, all had clinically meaningful improvements from baseline.
However, in a prespecified group of subjects with unilateral knee OA symptoms, and a post-hoc group with unilateral symptoms but no widespread pain, the drug gave a significant improvement in the WOMAC pain score.
It was safe and well tolerated. In a Phase IIb trial, 695 patients with moderate to severe knee OA were given 2 mL intra-articular injections containing 0.03, 0.07, 0.15 or 0.23 mg of the drug, a placebo or a dry needle sham.3
Those given 0.07 or 0.23 mg doses showed significant improvements in the pain numeric rating scale (NRS) at both weeks 12 and 24, with the 0.07 mg dose also giving significant improvements in the WOMAC pain and function scores after 12 weeks, and the 0.23 mg dose after both 12 and 24 weeks.
There was no significant difference from the placebo for the other doses. The optimal dose for future studies was determined to be 0.07 mg. The company has also recently completed two Phase III trials.
Preliminary results showed statistically significant and clinically meaningful improvements in joint structure as shown by X-ray results of the medial joint space width.
Final analysis of the results, released via press release, showed that the patients also had a statistically significant improvement in WOMAC pain scores at both months 6 and 12, and a significant improvement in WOMAC function scores at month 12.
In a second, shorter-term study, preliminary analysis indicated that it did not meet the primary endpoint of pain reduction at week 12, with an unusually high placebo response being observed. The company is analysing the results to determine why this occurred.
References
- V. Deshmukh, et al., Osteoarthritis Cartilage 27, 1347 (2019).
- Y. Yazici, et al., Arthritis Rheumatol. 72, 1694 (2020).
- Y. Yazici, et al., Osteoarthritis Cartilage 29, 654 (2021).
