Of the 50 new drugs approved by CDER in 2021, almost half were tablets and capsules (23 in total).1 Modern tablet production may date back to the 19th century, but the technology continues to challenge today’s formulators.
Offering unrivalled patient acceptability, convenience, shelf-life and ease-of-use, oral solid dosage (OSD) forms remain the most popular drug delivery vehicle; as such, extending their application is an important goal. Modified/sustained release, fixed dose combinations and oral biologics are increasingly prevalent within the OSD landscape.2
Dissolution testing is a central analytical tool in the formulation and manufacture of tablets and capsules. For OSD products, drug delivery begins with the release of the active ingredient(s) from the drug product matrix into solution.
This is the process into which dissolution testing provides insight, both with respect to the speed of drug release and solubility. As a result, it is used from early research and development (R&D) into quality control (QC) and for the demonstration of bioequivalence.
The relevance of dissolution testing
The dominance of tablets and capsules for drug delivery can be attributed to their appeal to drug manufacturers, clinicians and patients. OSD forms are relatively easily manufactured at high throughput — compared with alternatives — and have high chemical and physical stability.
An important benefit for clinicians is the ability to control the amount of drug delivered to the body via the prescription of a specific dose. These attractions create considerable impetus to maximise the use of OSD products by enhancing their applicability.

Dissolution testing is central to these efforts, providing information to support the use of increasingly sophisticated formulation strategies that often share the common goal of controlling the drug release profile. A brief survey of current OSD development and production trends helps to elucidate the evolving motivations and requirements for dissolution testing.
Sustained release: Our ability to precisely engineer OSD products that deliver drugs during an extended period, often with the goal of maintaining a consistent concentration in vivo, continues to advance. Polymeric tablet coatings are one of the simplest strategies, but capsules are also readily engineered for targeted or extended release.
More complex matrix and multilayer tablets are a growing focus. Two- and three-layer structures allow formulators to achieve both immediate and sustained therapeutic activity with a single dose containing one of more actives, while simultaneously minimising the risk of interactions between tablet components.3,4
Fixed combination: Combining actives in a single OSD is an important product lifecycle management strategy for pharmaceutical manufacturers that delivers streamlined regimens for patients. Over-the counter remedies for pain relief are a well-established commercial example and illustrate the benefits of delivering complementary actives in a single dose during different timeframes.

3D printing: The first 3D printed drug product, SPRITAM, was approved for use in 2015 and efforts are accelerating to explore the potential of this novel manufacturing technique.5 3D printed tablets have the potential to deliver large drug payloads rapidly — owing to their porous nature — and with minimal amounts of liquid. Opportunities for customisation and responsive localised manufacture are primary drivers of interest.
Personalisation: The personalisation of medicine is increasing demand for OSD forms that are customised to specific populations (patients of a certain age, gender or body mass index, or even for individuals).
Fixed combination strategies and 3D printing both have a role to play here, but so too do innovative dosage forms such as snap tab tablets that have designated break lines to allow precise fractional dosing. Capsules can be a straightforward, easily developed option for customised products and offer valuable flexibility for colour and size differentiation.6
Formulating poorly soluble actives: The use of high throughput screening and combinatorial chemistry in drug discovery have led to an increase in the proportion of poorly soluble drugs in the new drug pipeline.7,8 Indeed, BCS (Biopharmaceutics Classification System) Class 2 drugs — those defined as having low solubility and high permeability — are now estimated to account for 50–60% of the drug pipeline.7
Improving solubility, either the rate of dissolution or the standing concentration that can be maintained in vivo, is now a defining challenge for formulators targeting an acceptable bioavailability for new drug entities. Example strategies include the use of alternative excipients, micronisation and formulation as amorphous solid dispersions.6
Oral biologics: The oral administration of biologics is not yet feasible … but drug developers are getting closer. Biologics tend to be extremely sensitive to the physical and chemical conditions in the gastrointestinal (GI) tract. The risk of proteolysis is high and the intestinal epithelium presents a significant barrier to diffusion for these large molecules.
Enteric coatings, mucoadhesives and permeation enhancers are all part of the toolkit being applied to reach clinically acceptable performance.9
Clearly, these trends create a multiplicity of requirements with respect to dissolution testing. The aim may be to accelerate dissolution or retard it, to track one active or more, to measure release rates during a very short timeframe or long periods.
Despite that, dissolution test methods have remained remarkably unchanged for many years. Standard methods are sufficiently versatile and flexible to serve the industry’s evolving requirements and offer substantial opportunity to modify test conditions to reflect product use.
USP dissolution methods for OSD forms
Pharmacopoeial test methods for OSD products safeguard performance from storage through to drug delivery. Hardness and friability values are primary indicators of physical integrity and stability; they’re specified to ensure that tablets and capsules are delivered to the patient intact, that dosing is consistent and that the product has a practical shelf-life.
Disintegration testing characterises the initial in vivo breakdown of an OSD product, whereas dissolution testing tracks the transition of the resulting smaller particles into a solution that diffuses into the bloodstream. This capability makes dissolution testing the primary in vitro method to investigate and compare the bioavailability of different OSD forms; that is, the amount of drug that the product makes available to the body.
Dissolution data support the optimisation and control of drug release profiles and the assessment of bioequivalence for generic products; its use extends right through to QC for the confirmation of batch-to-batch equivalence. Ph. Eur. 2.9.3 and USP Chapter <711> detail the range of apparatuses and techniques that have evolved to meet dissolution testing requirements for different types of OSD products.
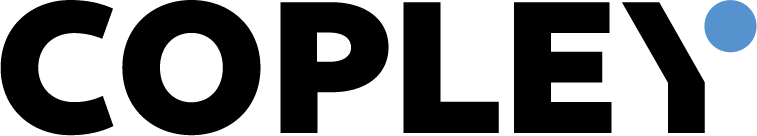
Figure 1 shows the most common apparatuses used for dissolution testing: Basket (Apparatus 1) and Paddle (Apparatus 2). Alternatives specified in the USP include Reciprocating Cylinder (Apparatus 3), Flow-Through Cell (Apparatus 4) and Reciprocating Holder (Apparatus 7). However, the use of these apparatuses tends to be restricted to highly specialised dosage forms.
Both Apparatus 1 and 2 utilise a dissolution tester, a cylindrical vessel that holds the dissolution media and is partially immersed in a water bath to maintain a (core body) temperature of 37 °C. With the Basket method, the OSD form is contained in a cylindrical mesh basket whereas, in the Paddle method, it simply sinks to the bottom of the vessel below the paddle.
Dissolution is promoted by rotation of the basket or paddle at a specified speed and samples of the dissolution media are extracted at predefined time intervals to track drug release. High performance liquid chromatography (HPLC) tends to be the technique of choice to quantify drug concentration. The resulting data are used to establish a dissolution profile — a plot of drug release as a function of time.
Multiple factors influence dissolution testing results. Some are necessarily controlled for accuracy whereas others are manipulated to improve the in vivo relevance of the data. Examples include the following.
Composition and deaeration state of the dissolution media: The composition of the dissolution media is varied to reflect the environment that the drug will be subjected to in the GI tract, to support decisions regarding whether a medication might be preferably taken with food or on an empty stomach and/or to assess how dissolution might change in different areas of the GI tract (particularly for extended release or sparingly soluble drugs).
Deaerating dissolution media prior to use helps to improve data integrity regardless of media composition as the presence of bubbles, notably on the surface of a sample but also on the test apparatus, can compromise accuracy by influencing permeability and/or buoyancy.

Physical dimensions of the test apparatus: Ensuring precise conformance with the pharmacopoeial specifications for dissolution testers is essential to confirm equipment suitability and safeguard accuracy. There are two ways to do this.
One is a technical check (mechanical or Enhanced Mechanical Calibration [EMC]) of the system’s physical dimensions; the other is to conduct a standardised test with a specific tablet (Performance Verification Test [PVT]). Standard PVTs are done using a prednisone tablet at a rotational speed of 50 rpm and assess far more than the physical dimensions of the vessels.
Systematic errors associated with media degassing and dosing, sampling, sample measurement and “human factors” can all have an impact, increasing the risk of false negatives.
Rigorous mechanical checks are more specific, with state-of-the-art practice involving half yearly EMCs as highly recommended by the FDA and ASTM.10,11 Such tests typically extend to, for example, the assessment of the verticality and centricity of agitation shafts as this can directly influence recorded data.
Temperature: Precise temperature control is critical for dissolution testing, notably for fast release products, for which experience suggests a 1 °C temperature difference can cause a variance in a dissolution profile of up to 10%. Avoiding temperature drops during sampling is important for data integrity.
Localised drug concentrations: In many instances, dissolution testing is done under sink conditions whereby it’s not inhibited by a high localised concentration of the drug substance. In certain circumstances, such as with certain actives and some extended-release products, these conditions may not be representative and/or may be difficult to achieve with a standard test set-up.
Modifying test conditions appropriately to address this issue is therefore essential.
Tablet surface area: Dissolution rate can change when a non-disintegrating tablet dissolves as this process naturally reduces the exposed surface area.
Accepting this phenomenon and measuring under conditions that allow it to happen may be the most relevant approach for a specific product; but, if not, then intrinsic dissolution testing can be done instead. This is a distinct method, which is particularly useful during early stage product development that determines drug release per unit surface area.
In summary, although dissolution testing is inherently simple, test conditions and methods require careful consideration to make in vitro in vivo (IVIV) relationships as robust as possible during R&D and to maximise sensitivity for QC.
Establishing a cost-efficient dissolution testing set-up
When it comes to establishing a dissolution testing set-up, selecting solutions that are robustly fit-for-purpose is critical for cost-efficiency. As discussed, having the flexibility to meet all requirements is essential … but unnecessary complexity can increase costs while delivering minimal benefit.
Bench space availability, the level of training needed to generate robust data and ongoing maintenance requirements can also be important and sometimes limiting factors.
Copley equipment for dissolution testing allows users to modify and control all the factors that influence data to maximise the utility of this core technique. The inherent simplicity of dissolution testing is reflected in testers that have clean lines and excellent visibility, are optimised for ease-of-use and benefit from precision, minimal maintenance and reliability.
Using these testers in combination with a thoughtfully curated range of accessories enables productive everyday testing from R&D through to QC. Copley DISi dissolution testers are available in a six or eight test station configuration.
The six-station system (the DIS 600i [Figure 2]) is one of the most compact dissolution testers available; the eight-station system (the DIS 800i [Figure 3]) is a higher capacity model for those that need it. Both testers offer full FDA, USP, Ph. Eur. (European Pharmacopoeia) and JP (Japanese Pharmacopoeia) compliance to the latest specifications, including
- intuitive touchscreen operation
- a broad range of rotational speed control
- centring systems for precise vessel positioning
- integrated temperature measurement and control
- extensive data reporting options and remote operation/control functionality
- sampling alerts that make it easier to implement predefined sampling regimes.
These dissolution testers can be used with either baskets or paddles to form Apparatus 1 or 2, respectively. The full Copley range also extends to USP Apparatus 5, USP Apparatus 6, an immersion cell and a suppository basket enabling the testing of a wide range of drug products.
Each individual test station has a basket and paddle that can be lowered independently for staggered starts and easy-to-clean membrane-sealed lids to minimise evaporative losses during testing; sampling probes can be tailored to both manual and automated requirements.
Key accessories for the dissolution testers include EMC Ultra Precision vessels, the Automated Tablet Drop and kits for intrinsic dissolution testing and low volume conversion.
EMC Ultra Precision vessels have dimensional tolerances that are approximately two times higher than those specified by the FDA, making them valuable for high accuracy testing. The Automated Tablet Drop guarantees simultaneous tablet ejection to make synchronised sampling easier while eliminating any requirement for time-lag correction factor calculations.
The accessory for intrinsic dissolution testing includes a punch and die kit and a hand-operated press that allow users to produce the tablets required, whereas the low volume accessory converts the 1000 mL standard dissolution tester vessel to either 100 or 200 mL.
Reducing the vessel volume can help to improve test accuracy when the drug concentration in the dissolution media is likely to be extremely low, such as when the OSD product contains low levels of drug and/or for extended-release testing.
In conclusion
For generic formulation and QC, dissolution testing is an essential part of the ongoing development of OSD products. Despite evolving product forms and trends in the properties of drug candidates for oral delivery, the core techniques and apparatus used for dissolution testing remain both simple and relatively unchanged.
For those investing in dissolution testing equipment, the key to cost-efficiency is to select systems with the flexibility required to reliably deliver accurate data for the product of interest. Copley’s dissolution testing range is precision engineered and designed with the insight that comes with delivering pharmaceutical testing solutions for more than seven decades.
Specified for productive everyday dissolution testing, it’s a cost-effective, high quality and robust choice for those looking to harness the potential of dissolution testing from R&D through to QC.
References
- fda.gov/media/155227/download.
- https://pharma-trends.com/2021/02/09/current-trends-in-oral-solid-dosage-forms/.
- M. Akhtar, et al., “Bilayer Tablets: A Developing Novel Drug Delivery System,” J. Drug Del. Sci. Tech. 60 (December 2020): 102079.
- M. Efentakis, et al., “Two- and Three-Layer Tablet Drug Delivery Systems for Oral Sustained Release of Soluble and Poorly Soluble Drugs,” Drug Dev. Ind. Pharm. 36(8), 903–916 (2010).
- aprecia.com/news/fda-approves-the-first-3d-printed-drug-product.
- F. Thomas, “Capsule Innovations: Speeding Up Drug Development,” Pharm. Tech. 44(9), 30–32 (2020).
- drug-dev.com/osd-formulations-dissolving-bioavailability-solubility-challenges-in-formulation-development/.
- M. Sherry Ku, “Use of the Biopharmaceutical Classification System in Early Drug Development,” AAPS J. 10(1), 208–212 (2008).
- pharmaceutical-journal.com/article/research/recent-advances-in-the-oral-delivery-of-biologics.
- fda.gov/regulatory-information/search-fda-guidance-documents/use-mechanical-calibration-dissolution-apparatus-1-and-2-current-good-manufacturing-practice-cgmp.
- astm.org/e2503-13r20.html.