Patients experience frequent pulmonary exacerbations that require antibiotic treatment and, often, hospitalisation. Symptoms include a chronic cough, the excessive production of sputum, shortage of breath and repeated respiratory infections.
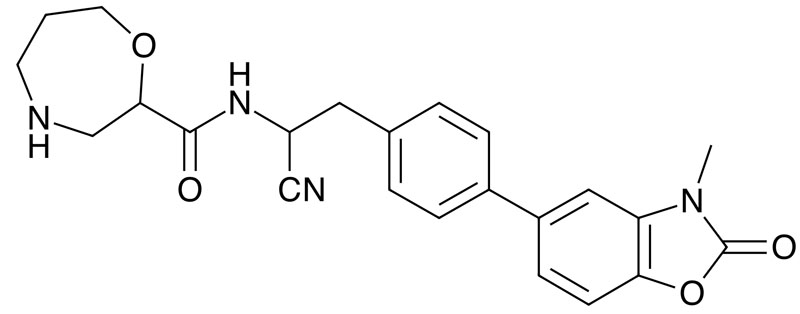
A potential treatment, brensocatib, is being developed by Insmed, having been in-licensed from AstraZeneca.1
It is a reversible inhibitor of dipeptidyl peptidase 1 (DPP-1), an enzyme that activates neutrophil serine proteases (NSPs) — including neutrophil elastase — in the neutrophils when they are formed in the bone marrow.
In chronic inflammatory lung diseases, these white blood cells accumulate in the airways, leading to excessive quantities of active NSPs.
The result is lung damage and inflammation. By inhibiting DPP-1 and thus preventing the activation of NSPs, it may be able to treat bronchiectasis and other neutrophil-mediated diseases.
After a successful Phase I trial, a randomised, double-blind, placebo-controlled study was done with 256 bronchiectasis patients who had had at least two exacerbations in the previous year.2,3
Subjects were given 10 or 25 mg of brensocatib or a placebo once a day for 24 weeks. The 25th percentile of the time to first exacerbation was 67 days with the placebo, 134 days with 10 mg and 96 days with 25 mg.
Both active treatments reduced sputum neutrophil elastase activity from baseline during the study period, whereas the incidence of adverse dental and skin events was higher than with the placebo.
Subsequent analysis indicated that neutrophil elastase activity was reduced in white blood cell extracts after 4 weeks of treatment with brensocatib in a dose-dependent manner.4
Positive results of a Phase III study have been announced via press release. In all, 1721 patients were given 10 mg, 25 mg or a placebo once a day for 52 weeks.
The primary endpoint was a reduction in the annualised rate of pulmonary exacerbations compared with the placebo, which was achieved by 21.1% of those given 10 mg of the drug and 19.4% with 25 mg; the drop in the rate of severe exacerbations was approximately 26% with both doses.
The prolongations of the time to first exacerbation were 18.7% and 17.5%, respectively, and the increase in odds of remaining exacerbation free were 41.2% and 40.0%.
It was well tolerated, with adverse events including nasopharyngitis, cough and headache.
The company is also investigating the drug’s potential in other neutrophil-driven inflammatory diseases. These include chronic rhinosinusitis without nasal polyps and hidradenitis suppurativa.
References
- K. Doyle, et al., J. Med. Chem. 59, 9457 (2016).
- H. Usansky, Clin. Pharmacol. Drug Develop. 11, 832 (2022).
- J.D. Chalmers, et al., New Engl. J. Med. 383, 2127 (2020).
- D. Cipolla, et al., Respir. Res. 24, 133 (2023).
